How can I treat epicondylitis?
The word epicondylitis derives from the word epicondyle (refers to an anatomical area of the arm bone, the humerus) + the suffix “itis”, which tends to designate some inflammation, in this case located in the elbow. In this type of pathology, one of the main symptoms is pain, which can be felt only in the elbow or along the forearm.
The American Society for the Surgery of the Hand defines epicondylitis as follows:
“Lateral epicondylitis, commonly known as tennis elbow, is a painful condition involving the tendons attached to the bone on the outside (side) of the elbow. (…).”
The pain is felt mainly over the bone on the outside of the elbow, where the upper arm muscles meet the forearm muscles. One of the main muscles involved in this condition is the common extensor of the fingers which, as its name suggests, stretches the fingers of the hand (see image below). Normally, several muscles that attach to the elbow and forearm region are involved.
The degeneration associated with the tendon insertion leads to this area being weakened and subject to greater stress. This fact can lead to pain, which appears in situations where this muscle is called upon, such as lifting weights, or situations in which we need to grab or pull something. I should mention that in scientific articles, the term most described and the most accepted name currently is “tendinopathy”, and not tendinitis, namely Lateral Elbow Tendinopathy (TLC), the name that will be adopted from here on.

TLC affects approximately 1% to 3% of the general population, with greater incidence and risk in people who smoke, manual workers and tennis players. This type of injury results in significant functional disabilitywith regard to work, sporting and leisure activities, and at the same time entails high costs due to loss of productivity and the use of healthcare.
We will soon make a video available on our youtube channel, with some stretches for the hand, wrist and forearm that can help relieve tension in the wrist flexor and extensor muscles.
The pathophysiology (the physiological and pathological reason) of TLC is multidimensional (diverse origins). On the other hand, there is strong evidence regarding the discrepancy between clinical severity and tendon pathology in patients with tendinopathy. This means that just by observing an examination it is not possible to assess the severity of the pain that the person may feel. It also means that there may be cases in which the person has severe pain but the examination does not show degenerative changes. In these cases, the changes may be related to other factors, such as changes in the peripheral nervous system (radial nerve), factors related to body biomechanics and possibly psychological factors.
Diagnosis of Lateral Elbow Tendinopathy
The diagnosis of TLC is essentially based on a clinical examination that aims to cause pain in the tendon affected by the load. Physical examination should reproduce pain in the lateral epicondyle area in at least 1 of 3 ways:
-
- palpation of the lateral epicondyle;
-
- resistance to extension of the wrist, index finger or middle finger;
-
- make the patient grasp an object.
The doctor monitoring the clinical case may consider it pertinent to carry out additional examinations, such as soft tissue ultrasound or even magnetic resonance imaging, however, according to the authors Coombes, Bisset and Vicenzino (2015) in a meta-analysis of MRI studies the authors found that 50% of those analyzed had visible tendon changes on MRI but had no symptoms.
In the same way, a study was carried out in which the tendons of individuals with tendinopathy were analyzed, but at the same time individuals without symptoms were used to carry out comparative ultrasound evaluations. The result of the study was that changes in the tendons were found in 90% of patients with TLC, but also in 53% of individuals who were asymptomatic. In other words, around half of the individuals without symptoms had tendon changes on ultrasound evaluation.
The exception was the case of rupture of fibrils within the common extensor tendon, in which case there was a 100% probability of elbow tendinopathy.
Conversely, negative ultrasound findings can be used to safely rule out lateral elbow tendinopathy as a diagnosis and prompt the physician to consider other causes of elbow pain.

Thus, given this imaging challenge, a more comprehensive physical examination may be necessary to identify (or rule out) coexisting pathologies or other reasons for the existence of pain. This is because an elbow is never just an elbow. The elbow is connected to the hand and shoulder more directly, as well as the spine. This explanation can be left for another article. What I want to communicate now is that in one of their books, Ellenbecker et al. (2013), point out that there are several studies that indicate that elbow tendinopathy is related to movement dysfunctions at the shoulder level, mainly with regard to joint ranges (and respective muscles) of internal and external rotation of the shoulder.
To simply measure and compare the internal rotation of the shoulder, we can make the movement of bringing the hand to the shoulder blade (for ladies, something similar to tightening/unfastening the bra). If the difference is significant or pain appears, it means that there is some change in the shoulder that needs to be evaluated, preferably before causing symptoms such as pain or limitation of movement in everyday life.
Thomas Myers, author of the theory of myofascial meridians, presents several lines or myofascial meridians that unite, in this case, the muscles of the elbow, forearm and shoulder.
In addition to the upper limb, as mentioned in one of the previous paragraphs, the evaluation of the cervical and thoracic spine and the function of the radial nerve should also be a priority, especially when there is concomitant neck pain, or diffuse pain in the arm, or paresthesia ( the familiar feeling of numbness). Reproduction of lateral elbow pain during manual palpation and/or active, passive or combined movements of the cervical spine should raise the suspicion of radicular or referred pain, in which case the cervical spine may need to be evaluated by an orthopedic doctor.
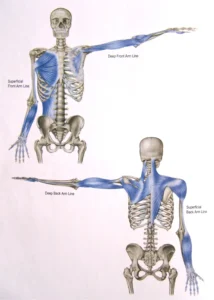
Many of us have suffered some type of pain in the shoulder, arm, elbow or even hand, due to the countless hours we spend at the computer. With this visualization of how these different muscles influence each other, it becomes easy to understand how a change in the shoulder and neck muscles can influence or increase pain and injuries at the elbow level, and vice versa.
If you don’t feel any type of pain, but work long hours at a desk or at the computer, believe me that it is still worth doing some exercises as a measure to enhance your well-being and the health of your muscles and joints, such as the demonstrated in the video above.
One of the things we get asked most about during consultations is about the best posture at the computer. We are saving this topic for another post to be published soon.
Is there treatment? What is the best approach?
Manual Therapy
Manual therapy techniques result in pain relief and improved grip strength.
There is also evidence that manual therapy techniques targeting the cervical and thoracic regions provide additional clinical benefits beyond local treatment of the elbow (…).
Exercise therapy
Exercise is fundamental to treatment, whether as the sole treatment modality or as part of a multimodal physiotherapy regimen (which makes use of manual therapies, therapeutic exercise and electrotherapy).
If the pain from tendinopathy is chronic (more than 6 months), exercise has been shown to lead to faster pain regression, shorter sick leave time, fewer doctor visits and greater work capacity.
Despite the clear benefits, the ideal intensity, duration, frequency and type of load for TLC rehabilitation have not yet been established. In general, the guidelines recommend applying a gradual increase in resistance, focusing on the wrist extensor muscles.
Given the variability of clinical presentation and the pathology itself, it is likely that optimal modes and doses of exercise will differ among patients with different stages or severity levels of tendinopathy.
Discipline
Those who study these matters guarantee that, most likely, the condition will resolve gradually with adequate rest and time.
Activities that cause pain should be avoided, ergonomic advice should be given to minimize work tasks that require postures with the wrist deviated, vigorous efforts and highly repetitive movements.
You should also gradually reintroduce more strenuous tasks and reduce the load on the tendon if it recurs, respecting your body’s limits.
Pharmacotherapy
The evidence is conflicting about the role of anti-inflammatories in the treatment of TLC.
There is strong evidence that corticosteroid medication provides short-term pain relief, but leads to worse outcomes after 6 and 12 months compared to a “wait and see” approach or physical therapy treatment, with rates of substantial recurrence.
Depending on the severity of the situation, a mixture of all these interventions may be necessary. In general, for moderate cases, a multimodal physical therapy regimen is recommended as first-line treatment, with the goal of faster pain reduction and recovery of function.
We suggest a minimum of 8 to 12 weeks of individually prescribed physical rehabilitation to target specific physical deficits, including progressive strengthening and resistance exercises and elbow manual therapy, consistent with what has been used in previous studies of tendinopathy side of the elbow.
Did you like this article? Share it with anyone who could benefit from this information or leave us a message.
Text based on the article Management of Lateral Elbow Tendinopathy: One Size Does Not Fit All

