
Do you usually feel pain in the front of your knee when you exert more effort, or when going down stairs or ramps?
Knee
When we talk about the knee, we must consider that it is a load-bearing joint, made up of 4 bones: tibia, fibula, femur and kneecap. We must bear in mind that, as it is a load-bearing joint, it is also a joint subject to many movements throughout the day, most of which we do not even realize we are doing.
There is a widely accepted theory that there are joints more prone to stiffness, and others more prone to instability, that is, there are joints that benefit more from mobility training, others from stability training. In the case of the knee, it is a joint that tends to suffer injuries due to instability and/or movement dysfunction, and therefore benefits from stability training. But it is not just the knee that matters, as We’ll see later.
Pain in the Front of the Knee
It’s one of the symptoms of a syndrome that affects many people, and there’s a justification for that: it’s called painful patellar syndrome (or patellofemoral syndrome).
Painful patellar syndrome (SRD) is typically characterized by pain felt behind the kneecap and described as being diffuse (Ferber et al., 2015; Neal et al., 2019). When the therapist questions, the person usually places their entire hand on top of the kneecap, and reports feeling this pain in activities that generate overload on the knee in flexion positions, such as going up and down stairs (Neal et al., 2019), and also jumping and running activities (Ferber et al.,2015).

In the general population:
-
- It affects around 15% to 25% of people (depending on the authors consulted)
-
- It is common in teenagers and adults
-
- It is mostly diagnosed in military personnel and athletes whose sport includes running (Ferber et al.,2015)
-
- It is a more typical pathology to be diagnosed in women than in men (relevance to anatomical and strength factors)
-
- More than 70% have recurrent or chronic pain in this joint, with an important psychological and emotional dimension in these cases, with some lack of understanding by their closest family circle
In a more recent study (2019), it is proposed that quadriceps weakness is the only considerable risk factor for the onset of SRD. Rejecting that the gender, age, body mass index, height, lower limb alignment, or hamstring and hip muscle strength are risk factors.
Role of the Physiotherapist
SRD has been studied for decades, and its treatment continues to be a challenge for both physiotherapists and exercise professionals. Even before the beginning of the second millennium, the relevance of SRD was studied. activation of the internal part of the quadriceps (vastus medialis and its oblique portion) at the origin of this pathology. Nowadays we know that to treat your complaints (person / patient) it is important not to limit ourselves to just treating the knee, but to integrate the knee into a continuum of movement and biomechanical analysis that integrates the entire body (foot, ankle, knee, hip and core).
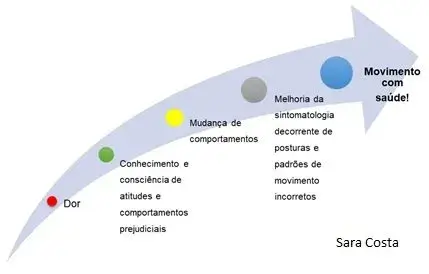
In the case of knee pathologies, specifically SRD but also for any pathology, the physiotherapist plays a very important role in clarifying and teaching the person/patient:
-
- Clear the person’s doubts regarding the medical diagnosis that may have already been made,
-
- Carry out the diagnosis in physiotherapy if there has not been a medical consultation, and refer if necessary,
-
- Evaluate, analyze and demonstrate which movements are most problematic for the pathology in question,
-
- Teach and demonstrate treatment and prevention strategies so that the person can take self-responsibility for the treatment (see figure 2.).
It was done um study in which they compared the effectiveness of a knee strengthening program VS knee and core strengthening, with a view to treating patellofemoral pain. In this study they concluded that:
-
- A 6-week strengthening program, with three weekly workouts, targeting the hip and knee resulted in significant improvements in pain, functional capacity and muscle strength
-
- For short-term treatment, the knee strengthening protocol, or knee strengthening protocol combined with hip strengthening, are equally effective
-
- The combined strengthening protocol generated faster improvements, as well as greater gains in overall muscular strength and core muscle endurance
6 Recommendations
Recently (2018) a consensus statement (by experts in the field) about exercise therapy and physical interventions, which resulted in the following 6 recommendations:
-
- Exercise therapy is recommended to reduce pain in the short, medium and long term, and improve functionality in the medium and long term.
-
- It is recommended to combine exercises for the hip and knee to reduce pain and improve functionality in the short, medium and long term, this combination being better than exercises targeting only the knee.
-
- Combined interventions are recommended to reduce pain in adults in the short and medium term. Combined interventions include exercise therapy combined with one of the following: plantar orthoses (insoles), patellar taping or manual therapy.
-
- Plantar orthoses (insoles) are recommended to reduce pain in the short term. In isolation, patellofemoral, knee or lumbar mobilization is not recommended. Electrophysical agents (as exclusive therapy) are not recommended.
Return to activity
Anyone who is limited in their activity, whether daily or sporting, due to pain or injury, has the question in their head “when can I return?”. This is true for the average person, who needs to know when they can return to their day-to-day life without restrictions (someone who works on their feet all day, or who needs to be present at meetings), but it is also especially worrying for top athletes who need to plan their presence at sporting events (or coaches, in the case of team athletes).
The following criteria are recommended to allow a return to sports:
-
- Absence of edema
-
- No pain when squatting or going up or down stairs
-
- Good quadriceps strength, especially vastus internus
-
- Adequate flexibility of the hamstrings
-
- Biomechanics of normal gait
-
- Adequate core stability strength
-
- Good performance in challenging functional tests
-
- The person feels ready and confident in the previously injured knee
If you liked this article, share it with anyone who could benefit from this information or leave us a message.






